In a previous article, we discussed how ultrasound-guided modified Seldinger technique combined with arterial catheterization can help address the challenge of arterial puncture in critically ill patients. Regarding arterial catheterization, a commonly performed clinical procedure, are there still some basic knowledge points and technical skills that need to be reviewed and consolidated? Today, we will study together a 2023 article published in the Emergency Medicine Australasia journal—“Arterial Catheterization.”
.png)
The article raised several core questions. Below is a summary and interpretation:
.png)
I. Indications
Primary: Continuous blood pressure monitoring (e.g., shock requiring vasopressors, aortic dissection, unreliable non-invasive blood pressure).
Secondary: Frequent arterial blood sampling.
II. Site Selection
First choice: Radial artery (easy access, good collateral supply, low complication rate).
Other options: Femoral, ulnar, brachial, dorsalis pedis, axillary, posterior tibial arteries.
Site characteristics:
Femoral: lower catheter failure rate (5%) compared with radial (30%), infection risk not necessarily higher.
Ulnar: tortuous course.
Brachial: lacks collateral circulation, severe complication rate 0.35% vs. radial 0.03%.
Distal radial: technically more difficult but not inferior to conventional radial access.
III. Contraindications and Complications
Contraindications: Proximal traumatic arterial injury, infection at puncture site, inadequate collateral circulation, coagulopathy.
Complications:
Rare but serious: ischemia with permanent damage (<0.1%), local infection (<1%).
Common: pain, paresthesia, bleeding, transient radial artery spasm (<50%), hematoma (15–50%).
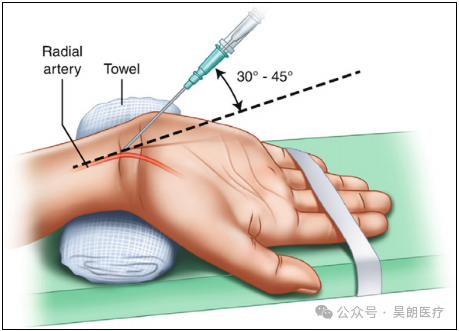
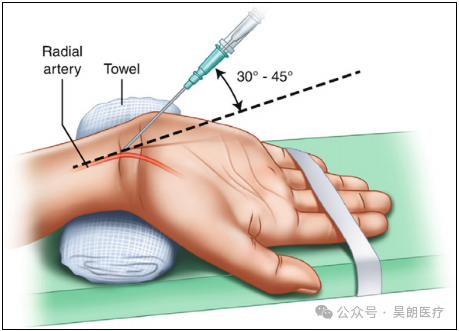
IV. Procedure
1. Equipment: Preparation items (rolled towel, tape), infection prevention (antiseptic, sterile drape, etc.), anesthetic (1–2% lidocaine), arterial catheterization kit, fixation materials.
2. Types of catheterization kits:
Conventional Seldinger (high first-attempt success).

Integrated modified Seldinger (fast, but failure requires discarding entire kit).

20G IV catheter (not recommended for routine use).

3. Patient positioning (radial artery): Recommended wrist extension at 45°; >60° decreases success rate.
4. Adjuncts: Ultrasound is first-line in difficult cases; real-time guidance is superior to pre-procedural skin marking.
5. Local anesthesia: In awake patients, 1–2 mL of 1% lidocaine; no evidence that lidocaine causes vasospasm or obscures the artery.
6. Pharmacologic adjuncts: No clear evidence supports systemic drugs before insertion to improve palpation.
7. Fixation: No gold standard; institutional protocols recommended. Routine suturing not advised.
8. Sterility requirements: At minimum—sterile gloves, sterile drape, skin antiseptic. For central sites, full barrier precautions are required.
V. Post-procedural Considerations
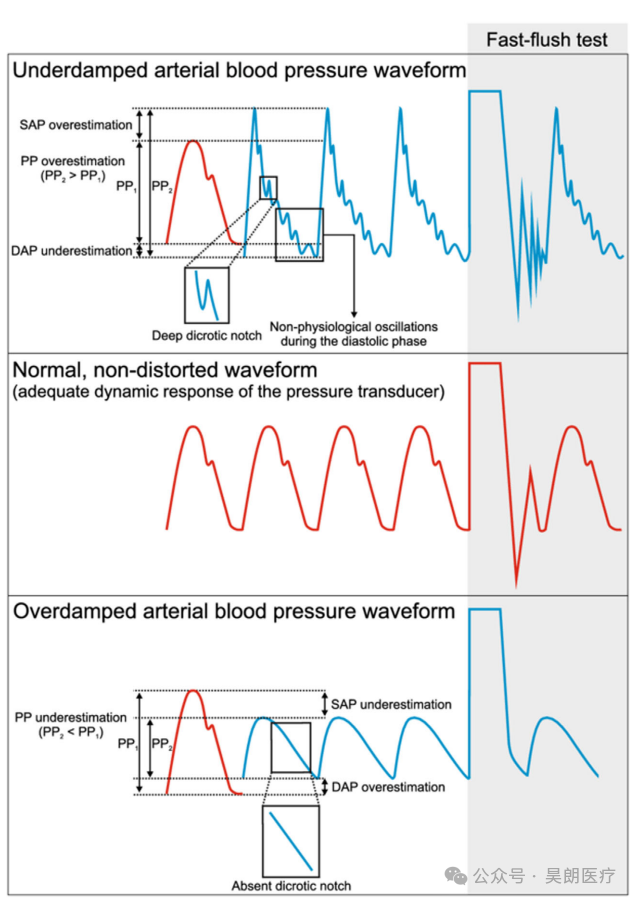
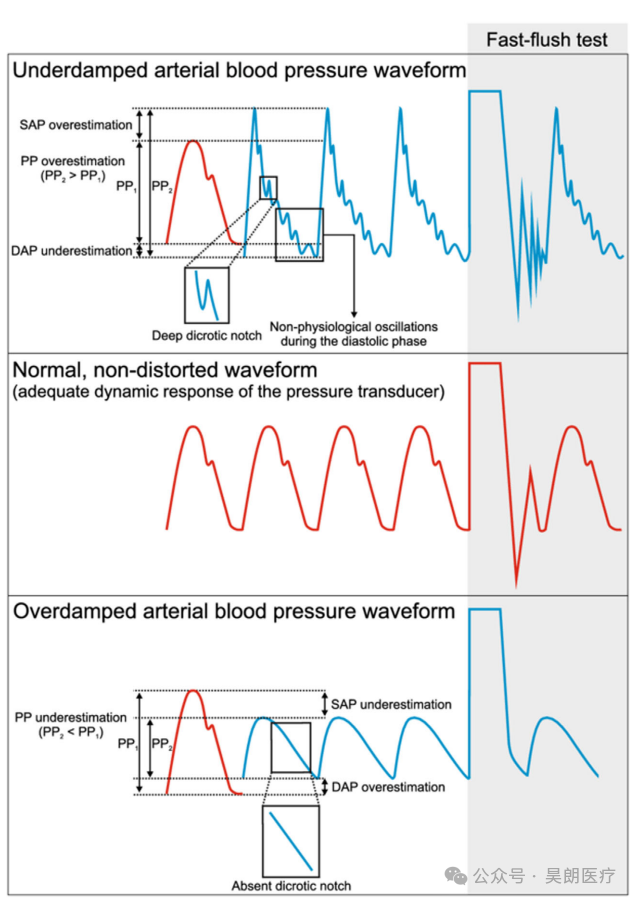
1. Waveform interpretation and troubleshooting:
Transducer should be leveled at the heart (≈5 cm below the sternum in supine patients). Mis-leveling leads to under- or overestimation of pressures.
Underdamping: overestimates systolic, underestimates diastolic, narrow peak waveform with deep dicrotic notch; causes include stiff tubing or faulty transducer. Mitigation: use short/stiff tubing, minimize stopcocks, avoid modifying pre-packaged kits, or use commercial systems.
Overdamping: underestimates systolic, overestimates diastolic, narrowed pulse pressure, blunted upstroke, absent dicrotic notch. Causes: low flush-bag pressure, bubbles, thrombus, kinking, loose connections. Troubleshooting: adjust wrist, ensure catheter patency, inspect tubing/connectors, flush to clear thrombus/air, consider tubing or catheter replacement. Distinguishing under- vs. overdamping: perform rapid flush/“square wave” test and observe oscillations.
2. Catheter removal:
Evidence suggests routine replacement is not recommended. Removal is indicated when ≥1 clinical sign of catheter-related bloodstream infection (CRBSI) is present (e.g., high fever), or when catheterization is no longer required.
3. Post-removal care: Apply manual pressure for 10 min (longer for femoral site or anticoagulated patients); inspect catheter integrity; monitor neurovascular status of limb for 15 min.
VI. Pediatric Considerations
1. Catheter size: <10 kg: 22/24G; 10–40 kg: 22G; >40 kg: adult sizes.
2. Puncture sites: May also include temporal artery, umbilical artery.
3. Adjuncts: Ultrasound guidance and guidewire use recommended (improves first-attempt success).
4. Complications: Overall low incidence (0.2%); higher femoral complication rates in infants and neonates.
VII. Key Conclusions
Serious complications are rare.
No evidence that arterial catheterization improves mortality or morbidity.
Allen’s test is not recommended for predicting collateral circulation adequacy or complication risk.
Use of heparinized saline in pressure bags does not prevent thrombosis.






.png)
.png)