In the field of critical care medicine, arterial catheters are the core means of hemodynamic monitoring. However, there has been a long-standing controversy regarding their replacement strategy. An evidence-based practice study published in the Journal of Nursing (Guo Hanhua et al., 2021) has provided a scientific basis for the standardized management of arterial catheters by integrating the best evidence. The key contents are analyzed from four aspects, namely the research background, core evidence, practical effectiveness and clinical value as follows:
I. Research Background: Breaking the Tradition of "Regular Replacement" and Exploring the Optimal Strategy Based on Evidence
Clinical Current Situation: There is a controversy regarding the routine replacement time of arterial pressure monitoring catheters. Some guidelines recommend replacement within 7 days. However, the CDC guidelines in 2011 and the Sydney guidelines in 2014 indicate that there is no need for routine replacement for the prevention of infection, and it should be evaluated as needed.
Core Question: Can the indwelling time be extended through evidence-based practice? How to balance the risk of infection and patient safety?
II. Evidence-based Process: Scientific Construction from Literature Screening to Review Criteria
1. Evidence Retrieval and Screening
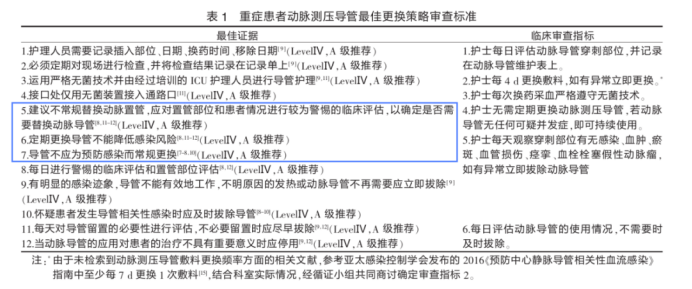
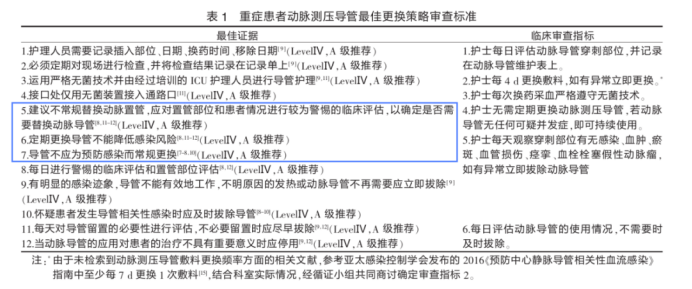
Eleven databases such as EMbase, PubMed, and Cochrane were searched. Three guidelines, two evidence summaries, and one randomized controlled study were included. Eventually, 12 items of the best evidence were formed and refined into six clinical review criteria (Table 1):
2.Intervention Measures
Tool Innovation: Self-made "Maintenance Form of Arterial Pressure Monitoring Catheter" is used to standardize the recording of the indwelling days, complications, and maintenance operations (Table 2):
.png)
Training and Supervision: Carry out special training, incorporate the strategy into the daily process, and have it supervised and implemented by the evidence-based team.
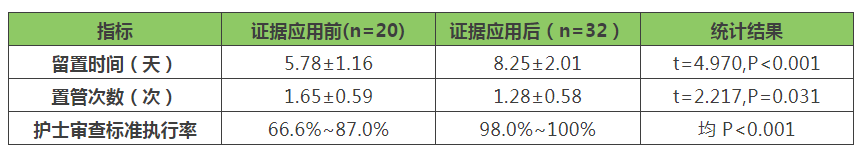
III. Practical Effectiveness: Validate the Safety and Effectiveness of the Strategy with Data
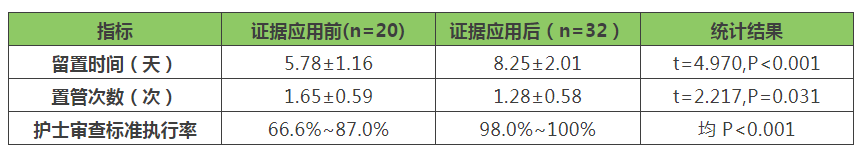
Key Findings:
(1)Extension of Indwelling Time: Through daily assessment instead of regular replacement, the average indwelling time of the catheter has been extended by 2.47 days, and there is no increase in the risk of complications such as bleeding, catheter blockage, and infection;
(2)Reduction in the Number of Catheter Insertions: The number of catheter insertions has decreased from 1.65 times to 1.28 times, reducing the vascular injury caused by repeated punctures and the patient's pain;
(3)Improvement in Nursing Standardization: The implementation rate of the six review criteria has reached over 98%, significantly improving the homogenization level of clinical operations.
IV. Clinical Significance: The Practical Transformation from Empirical Medicine to Evidence-based Medicine
1.Update of the Concept of Infection Prevention and Control: It has been confirmed that the strategy of "replacement as needed" does not increase the risk of infection, overthrowing the traditional understanding of "regular replacement for infection prevention", which is consistent with the CDC guidelines in 2011;
2.Double Improvement of Patient Safety and Efficiency: Extending the indwelling time reduces vascular injury and lowers medical costs (reducing catheter consumption and the time of puncture operations);
3.Quality Improvement Paradigm: Through the evidence-based nursing model (JBI Evidence Application Framework), the best evidence is transformed into actionable review criteria, providing a replicable practical path for the management of catheters in the ICU.
V. Research Limitations and Future Directions
Although the study has confirmed the effectiveness of the strategy, due to the single-center sample size (52 patients) and the complexity of ICU patients, multi-center studies are needed for further verification. In the future, ultrasound-guided puncture and intelligent monitoring technologies can be combined to continuously optimize the full-cycle management of arterial catheters.
Conclusion
This study provides an "evidence-based precise strategy" for the management of arterial pressure monitoring catheters in critically ill patients: determining the replacement timing through daily clinical assessment instead of mechanical regular replacement. This practice not only improves the standardization of nursing care but also proves the feasibility of "safely extending the indwelling time" with data, laying an important foundation for promoting the refined management of invasive procedures in the ICU.
Reference:
Guo Hanhua, Chen Minggui, Kong Lili, et al. Evidence-based Practice of the Optimal Replacement Strategy for Arterial Pressure Monitoring Catheters in Critically Ill Patients [J]. Journal of Nursing, 2021, 28(02): 37-41. DOI: 10.16460/j.issn1008-9969.2021.02.037.






.png)